Superfund Research Program
Protein Provides Insight into Respiratory Toxicity of Cadmium
View Research Brief as PDF(421KB)
Release Date: 05/04/2022
![]() subscribe/listen via iTunes, download(5.5MB), Transcript(87KB)
subscribe/listen via iTunes, download(5.5MB), Transcript(87KB)
A protein called fibrinogen can be an indicator of cadmium exposure in people with chronic obstructive pulmonary disease (COPD), according to a study led by Veena Antony, M.D., director of the NIEHS Superfund Research Program (SRP) Center at the University of Alabama, Birmingham. COPD stems from thickening of airways in the lungs, resulting in shortness of breath and persistent coughing.
Sources of cadmium exposure include cigarette smoke and emissions from industrial activities, such as fossil-fuel burning and smelting.
Cadmium exposure is associated with COPD, and research has also shown that people with COPD have higher levels of fibrinogen. Through a series of human and mouse studies, Antony's team explored potential connections between fibrinogen and cadmium in people suffering from COPD.
Measuring Cadmium
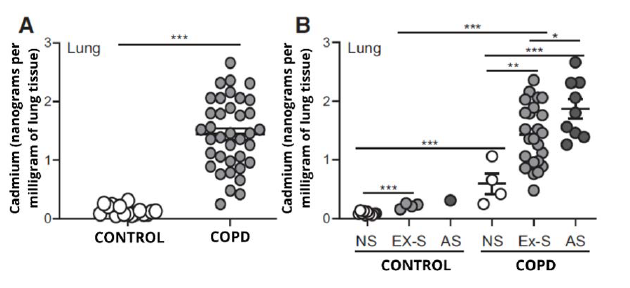
Using a technique that detects trace metals in biological samples, the researchers analyzed lung tissue from volunteers with and without COPD.
They found that cadmium content was much higher in participants with COPD compared to healthy participants. Among those with COPD, cadmium levels were highest in smokers.
In addition, samples from people with COPD who had never smoked contained more cadmium than lung tissue from healthy participants with no smoking history. The findings suggested that cigarette smoke was not the only source of cadmium exposure in those living with COPD.
Finding Fibrinogen
Antony and colleagues next examined fibrinogen levels in participants with COPD.
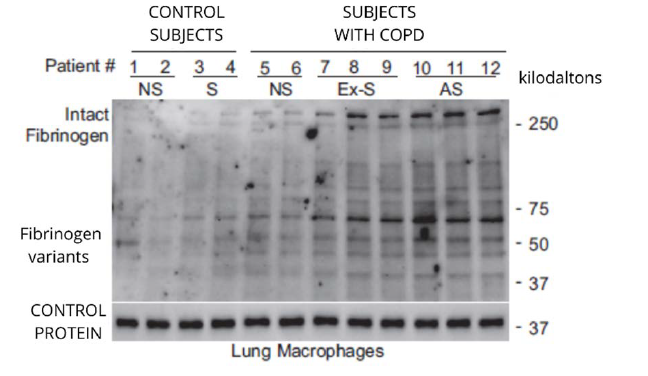
The team collected lung macrophages — immune cells that are first to activate when toxins like cadmium are inhaled — from volunteers, then studied their contents using a method that separates target proteins by mass.
Results showed high fibrinogen concentrations in macrophages from those with COPD.
Levels of fibrinogen also correlated with the levels of cadmium measured earlier. In other words, people with more cadmium had more fibrinogen, too.
Further, participants with more fibrinogen performed worse on a standard breathing test of lung function.
Unraveling a Chain of Events
To better understand the molecular ties between fibrinogen and cadmium, the team treated macrophages from participants with COPD to a solution containing dissolved cadmium. They found that cadmium stimulated the immune cells to make fibrinogen, as well as PAD2, a protein previously observed to occur at high levels in people with COPD.
The finding suggested a possible relationship between PAD2 and fibrinogen. To test that idea, the researchers used a technique to prevent the macrophages from making fibrinogen, then again administered the cadmium solution. They found that PAD2 levels decreased when fibrinogen was absent.
Mouse studies revealed more insight. The team first induced COPD-like symptoms in two strains of mice — one that could produce PAD2 and one that could not. Then they extracted lung macrophages, treating them to a solution of cadmium, fibrinogen, or both. The metal-protein combination caused an increase in cellular signals known to activate macrophages, but only in the mice that could make PAD2.
As the researchers noted, cadmium might activate macrophages, with fibrinogen playing a middle-man role in the presence of PAD2. The implications are important because abnormal macrophage activity can contribute to the inflammation characteristic of COPD.
Additional mouse studies showed that cadmium and fibrinogen can also promote accumulation of proteins that, at certain levels, can also contribute to lung damage.
For More Information Contact:
Veena Antony
University of Alabama at Birmingham
Division of Pulmonary, Allergy and Critical Care Medicine
1900 University Blvd
Birmingham, Alabama 35294-0006
Phone: 205-975-3258
Email: vantony@uab.edu
To learn more about this research, please refer to the following sources:
- Li FJ, Surolia R, Singh P, Dsouza K, Stephens CT, Wang Z, Liu R, Bae S, Kim Y, Athar M, Dransfield MT, Antony V. 2022. Fibrinogen mediates cadmium-induced macrophage activation and serves as a predictor of cadmium exposure in chronic obstructive pulmonary disease. Am J Physiol Lung Cell Mol Physiol doi:10.1152/ajplung.00475.2021 PMID:35200041
To receive monthly mailings of the Research Briefs, send your email address to srpinfo@niehs.nih.gov.


