Superfund Research Program
September 2021
Involving the community is valuable when adjusting clinical and public health guidance, especially as it relates to the health effects of per- and polyfluoroalkyl substances (PFAS) and other chemicals of concern.
NIEHS Superfund Research Program (SRP)-funded researchers were part of an ad-hoc committee that met six times between February and August to hear the experiences of communities across the country affected by exposure to PFAS and use that information to help shape new recommendations.
Appointed by the National Academies of Sciences, Engineering, and Medicine (NASEM), the committee is now tasked with reviewing the lessons learned from these sessions to recommend changes to clinical guidance so individuals exposed to PFAS could best be served by healthcare providers. NASEM is providing the Centers for Disease Control and Prevention (CDC) and NIEHS with:
- An objective review of current evidence regarding health outcomes associated with PFAS exposure.
- Recommendations for changes to the CDC PFAS clinical guidance.
“The goal was to hear the perspectives of people from all around the U.S., including Pacific Islanders and other disproportionately affected communities,” said Northeastern University SRP Center researcher Phil Brown, Ph.D. “This shed light on the similarities across different regions, the issues they are facing, and their concerns.”
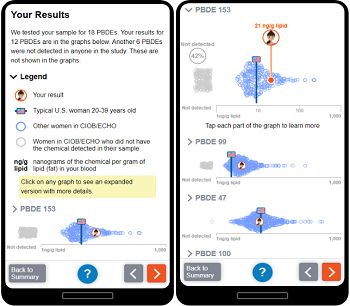
DERBI provides data on personal exposure to a myriad of chemicals, including phthalates, phenols, and pesticides, and allows participants to compare their results with others in the study and U.S. averages.
(Photo courtesy of Julia Brody)
The meetings focused on understanding the most critical needs of communities exposed to PFAS and the best strategies to ensure their well-being. Community representatives and other stakeholders shared their experiences and perspectives.
Scientists and clinicians shared lessons learned from working closely with PFAS-affected communities. For example, Julia Brody, Ph.D., from the Northeastern University SRP Center and Silent Spring Institute, talked about the importance of reporting back clinical results in a timely manner. Brody introduced Silent Spring’s Digital Exposure Report-Back Interface (DERBI), which Northeastern leveraged to share exposure and biomonitoring data with study participants.
Brown, Jamie DeWitt, Ph.D., from the North Carolina State University SRP Center, and Rainer Lohman, Ph.D., director of the University of Rhode Island SRP Center, were among the community liaisons who helped link community representatives and the NASEM committee.
Informing decision-making
Through these conversations, community liaisons identified critical actions needed for affected communities, including testing for PFAS in blood samples, improved education for healthcare providers, and increased attention on vulnerable communities and occupational exposures.
“Overwhelmingly, community members want their exposures and potential health risks to be taken seriously,” said DeWitt. “They would like to have more information about their exposure levels and how to prevent adverse health effects.”

Attendees spoke of difficulties faced by environmental justice communities and populations of concern that had not been considered before, such as people working in textile factories and food services. Many communities struggling with PFAS contamination face multiple challenges, including other contaminants in their drinking water and lack of access to healthcare providers.
“We learned that the most urgent need is to implement blood testing for PFAS as part of routine preventive healthcare in communities with known sources of PFAS contamination,” said Brown. “This also means that we need to provide more comprehensive education on environmental health for physicians to be able to answer patient questions and establish a plan to monitor their health.”
Other SRP-funded researchers who are part of the committee include Melissa Gonzales, Ph.D., of the University of New Mexico SRP Center, Erin Haynes, Ph.D., of the University of Kentucky SRP Center, Jane Hoppin, Ph.D., of the North Carolina State University SRP Center, and Tamarra James-Todd, Ph.D., of the Harvard School of Public Health SRP Center.


